Running Injury Spotlight
IT Band Pain: What It Really Is and How to Manage It Effectively
Derek Lam Physical Therapy and Performance | Oakland, CA
If you’ve ever experienced pain on the outside of your knee—especially during or after running—you may have heard about the iliotibial (IT) band. Long believed to be a culprit due to "tightness" or "friction," our understanding of this structure has significantly evolved. Let’s break down what the IT band actually is, why it might hurt, and how you can treat it effectively with strategies rooted in current evidence.
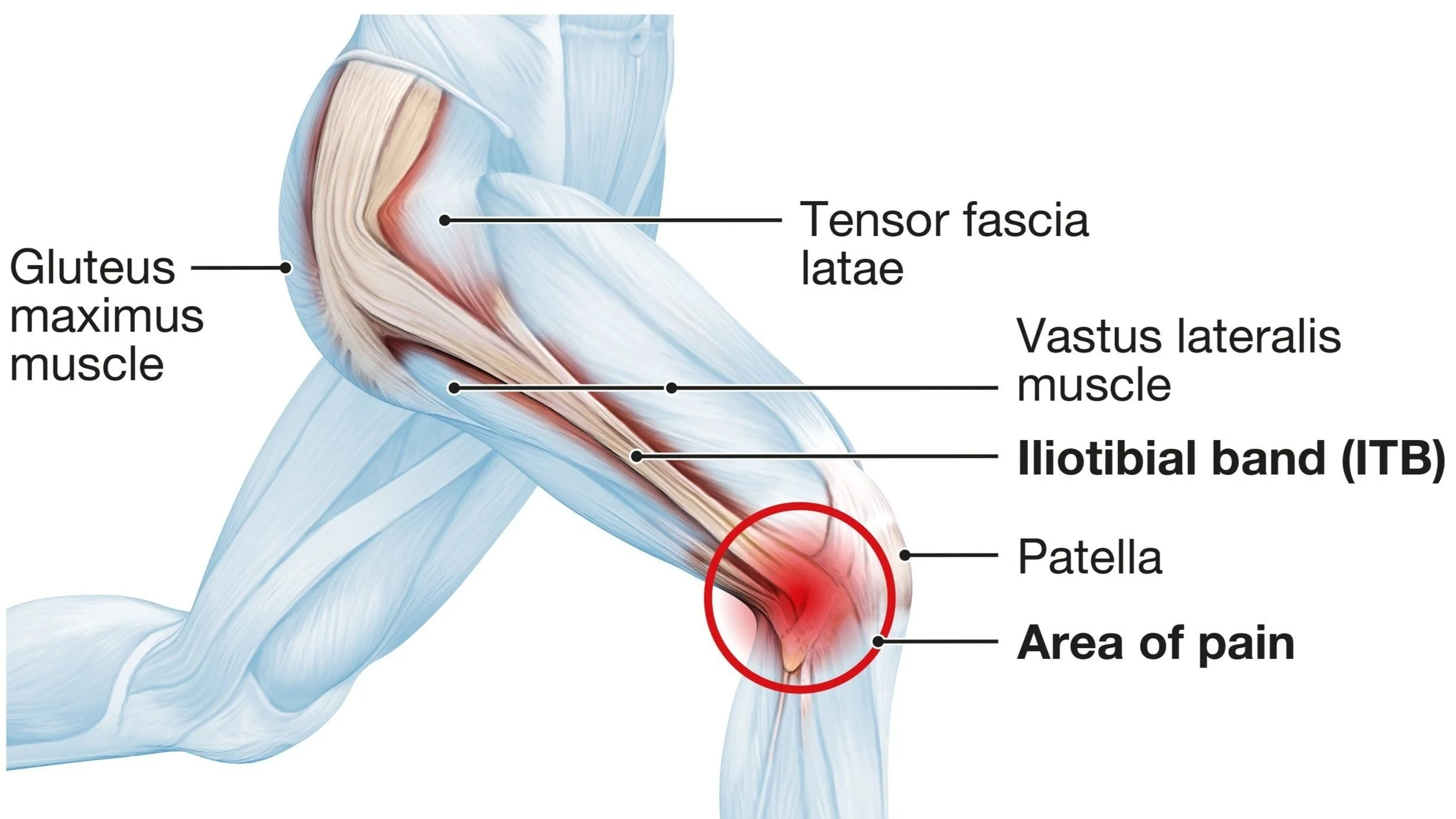
Anatomy of the IT band showing knee and hip connection
IT Band 101: Structure and Function
The IT band is a thick strip of connective tissue that runs along the outside of your thigh. It connects the pelvis (ilium) to the shinbone (tibia) and integrates fibers from both the tensor fasciae latae (TFL) and gluteus maximus muscles. Rather than being a standalone muscle or tendon, it's an extension of the fascia lata, a sheath that surrounds the thigh like a compression sleeve.
Its main roles include:
Assisting with hip and knee stability
Helping the body store and release energy efficiently during walking and running
Busting the Myth of “Friction Syndrome”
For decades, lateral knee pain was often labeled as IT Band Friction Syndrome, based on the idea that the band rubbed over a bony point on the thighbone (the lateral femoral epicondyle). This theory led to common treatments like:
Stretching to “lengthen” the band
Foam rolling to “break up adhesions”
Positive Ober’s test results being interpreted as “tightness”
However, updated anatomical studies show that the IT band is securely anchored to the femur, meaning it doesn’t glide back and forth. The sensation of “movement” is actually due to varying tension in different parts of the band during knee motion—not literal friction.
What’s Really Causing the Pain?
Current thinking suggests that sensitive tissue beneath the IT band, such as fat pads or connective tissue, may be compressed during repetitive motion—especially between 20–30° of knee flexion. This often occurs in runners, cyclists, or hikers who’ve had a sudden increase in training load.
This concept aligns with the idea of an “envelope of function”—a framework used to describe how much load your joints can safely handle. When you push beyond your current capacity (e.g., doubling your running distance too quickly), the body may not be able to adapt fast enough, leading to pain or irritation.
Managing IT Band-Related Pain: A Smarter Approach
1. Adjust Your Training Load
Rather than completely stopping activity, scale back to a manageable level. You may need to reduce:
Running volume (weekly mileage)
Intensity or frequency (speed work)
Time spent on uneven terrain or downhill slopes
Cross-training (e.g., cycling, swimming, or elliptical) can help maintain cardiovascular fitness while reducing strain on the IT band.
2. Try Gait Adjustments
Research shows that small tweaks in your running mechanics may help reduce IT band stress. Specifically:
Increasing cadence by 5–10% can reduce hip adduction and strain on the lateral knee
Shorter strides and slightly wider steps improve biomechanics and decrease pressure on the IT band
Use apps or wearable tech (like a Garmin) to monitor cadence during runs.
3. Strengthen Key Areas
Targeted resistance training is crucial—especially for the hips, quads, hamstrings, and calves. Even if weakness isn’t the root cause of your symptoms, strengthening these areas can improve your capacity and resilience to load.
Aim for 2 strength sessions per week, which can be programmed the same day as running days if your schedule allows. Progress gradually over 3–6 months.
Sample Exercise Progressions:
Quad-Focused:
Split squat holds → Rear foot-elevated split squats → Deficit variations
Step-ups → Lateral and forward step-downs
Hamstring-Focused:
Long lever bridges → Sliders → Nordic curls
Glutes and Hip Stabilizers:
Side planks → Hip lifts
Crab walks → Fire hydrant holds
Calves:
Double- and single-leg heel raises, progressing to weighted step work
Each progression is scalable—start with what’s tolerable and build from there. Slight discomfort (around 2/10 pain) during exercises is generally acceptable as long as symptoms don’t worsen over time.
Takeaways
IT band pain is not caused by friction or tightness.
The primary driver is often a training error or a spike in activity beyond your current capacity.
Load management, running form adjustments, and progressive strength training are your best tools for recovery.
Passive treatments like aggressive foam rolling or stretching are less effective than strategic movement and strength work.
Ready to Move Better?
If you're dealing with IT band pain or want help building a custom rehab or running plan, schedule a visit at Derek Lam Physical Therapy and Performance. I offer personalized, evidence-based care to help you get back to the activities you love—stronger and smarter than before.
Ready to book your first visit with me? Visit www.derekorthopt.com or click here to schedule online. I’m here to help you get back to doing what you love—pain-free.
📍 Derek Lam Physical Therapy and Performance
🏢 399 Grand Ave, Oakland, California 94109
🌐 www.derekorthopt.com
📆 Book Online Now